Do you often experience a burning sensation in your chest or throat after meals, or when lying or bending down? If so, then you are likely amongst the 25% of the UK population suffering from ‘heartburn’ caused by acid reflux or its more chronic form of GERD (Gastroesophageal reflux disease).
While medications like Omeprazole, Lansoprazole, and Pantoprazole (Proton Pump Inhibitors or PPIs) can offer short-term relief, prolonged reliance on these drugs does not address the root cause. In fact, suppressing stomach acid with PPIs can compromise digestive health and hinder your body’s ability to absorb essential nutrients and protect itself from pathogens.
Let’s dive into why acid reflux occurs, the positive and negative effects of PPIs, and natural ways you can manage and prevent heartburn through nutrition and lifestyle.
Acid reflux is an extremely common digestive condition affecting as many as 1 in every 4 adults in the UK.
What Is Acid Reflux?
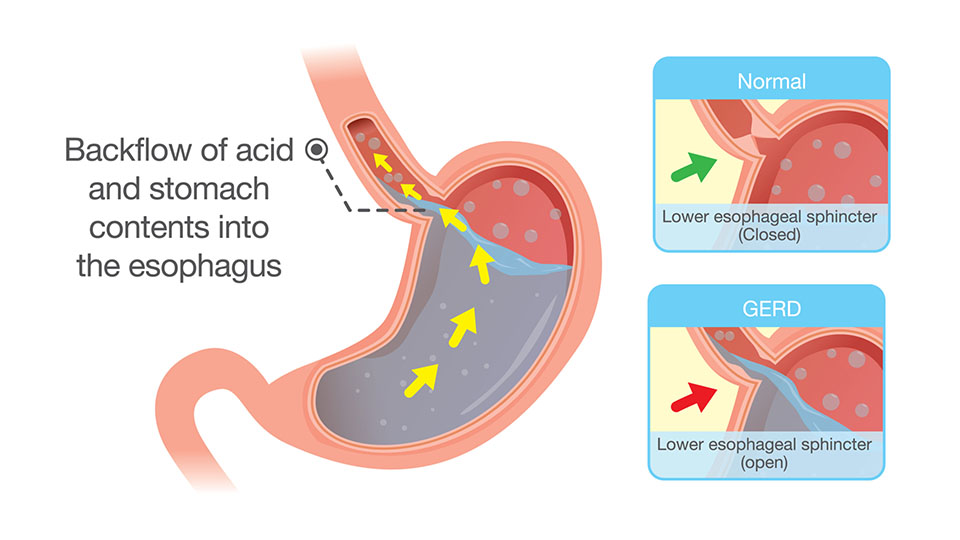
Acid reflux occurs when stomach contents including gastric acid flow back into the oesophagus, resulting in a burning sensation in the chest and throat. Several factors can contribute to the development of acid reflux:
▪️ Certain Foods and Beverages: Spicy or fatty foods, citrus fruits, tomatoes, chocolate, caffeine, and alcohol can trigger acid reflux in some individuals.
▪️ Weak Lower Oesophageal Sphincter (LES): The LES is a ring of muscle that separates the oesophagus from the stomach. If it weakens or relaxes, it allows stomach acid to flow back into the oesophagus.
▪️ Overeating: Consuming large meals or lying down right after a meal can increase the likelihood of acid reflux.
▪️ Being Overweight or Pregnant: Excess weight, especially around the abdomen, can put pressure on the stomach and contribute to acid reflux. Pregnancy can also lead to increased pressure on the stomach.
▪️ Smoking: Tobacco smoke can weaken the LES and contribute to acid reflux.
▪️ Certain Medications: Some medications, such as antihypertensives, antihistamines, and certain asthma medications, may relax the LES or irritate the oesophagus, leading to acid reflux.
▪️ Medical Conditions: Conditions such as hiatal hernias, scleroderma and diabetes can affect the function of the oesophagus and increase the risk of acid reflux.
Should I Take Proton Pump Inhibitors (PPIs) For Acid Reflux?
Proton pump inhibitors (PPIs) are a class of medications commonly used to reduce excess stomach acid production. PPIs work by blocking the enzyme in the stomach lining that produces acid, thus reducing the amount of acid produced.
Commonly prescribed PPIs include omeprazole, esomeprazole, lansoprazole, pantoprazole, and rabeprazole. PPIs are generally recommended by a doctor when you are suffering from:
1. GERD (Acid Reflux)
PPIs are often prescribed as a short-term solution to reduce stomach acid production, allowing the oesophagus to heal and repair from the effects of heartburn.
2. Gastric Ulcers
Occur when excessive stomach acid damages the inner lining of your stomach. PPIs can help heal and prevent ulcers that form as a result of taking non Steroidal Anti-inflammatory drugs (NSAIDs).
3. H. pylori
PPIs are prescribed as they lower the stomach acidity and allow antibiotics to work more effectively and eliminate harmful bacteria.

Book a Free Discovery Call
Discuss your health concerns with one of our expert practitioners and find out how personalised functional medicine can get your health on the right track.
What Are The Risks Of Taking PPIs?
While PPIs can be effective in managing acid-related conditions, they do not treat the underlying cause of acid reflux, and long-term use can have knock-on effects for your health and cause other detrimental conditions:
▪️ Rebound Acid Hypersecretion: Prolonged use of PPIs can lead to an increase in stomach acid production when the medication is discontinued. This phenomenon, known as rebound acid hypersecretion, may result in a recurrence or worsening of acid-related symptoms.
▪️ Nutritional Deficiencies: Stomach acid plays a role in the absorption of certain nutrients, such as calcium, magnesium, and vitamin B12. Reduced stomach acid production due to PPI use may lead to deficiencies in these nutrients over time.
▪️ Increased Risk of Infections: Stomach acid serves as a barrier against ingested pathogens. PPIs may reduce this protective effect, potentially increasing the risk of gastrointestinal infections such as Clostridium difficile (C. difficile) and pneumonia.
▪️ Bone Fracture Risk: Some studies suggest a possible association between long-term PPI use and an increased risk of bone fractures, particularly in the hip, spine, and wrist. The mechanism behind this association is not fully understood.
▪️ Kidney Disease: There have been reports linking long-term PPI use to an increased risk of kidney disease. However, more research is needed to establish a clear causal relationship.
▪️ Interactions with Other Medications: PPIs may interact with certain medications, affecting their absorption and effectiveness. It’s essential to inform healthcare providers about all medications being taken to avoid potential interactions.
▪️ Cost: PPIs can be relatively expensive, especially in some regions or without insurance coverage, making long-term use a financial consideration.
What Is The Best Way To Discontinue PPIs?
Doing so gradually and under medical supervision to minimise the risk of rebound acid hypersecretion and recurrence of symptoms is essential. Keep in mind that it’s usual to continue experiencing symptoms of reflux for about 2 weeks after you stop the medication. The following strategies can help calm reflux symptoms until rebound hyperacidity is resolved:
▪️ Slowly Taper Off PPIs: Reduce intake over 2-4 weeks (the higher the dose, the longer the taper).
▪️ Focus On Nutrition: Avoid alcohol, caffeine, chocolate, cow’s milk, high fat foots, and orange juice.
▪️ Practice Relaxation: Deep breathing enhances vagal stimulation, encouraging digestion and aiding peristalsis.
How Can I Treat Acid Reflux Naturally?
✅ Improve Your Gut Health
The healthier your gut microbiome, the better your digestive function and the less likely you are to experience acid reflux. Improve your gut health to address the root causes of gut complaints and acid reflux.
✅ Consider Functional Testing
When suffering from digestive symptoms such as acid reflux for a prolonged period, it’s essential to get to the root cause and identify or rule out underlying health conditions.
Stomach acid and heartburn can be symptoms of gut infections or dysbiosis (an imbalance in your gut microbiome). The H pylori bacteria is a common culprit behind gut infections and can lead to stomach ulcers, gallbladder issues, heartburn.
Our comprehensive stool tests accurately pinpoint imbalances or pathogens in your system.
✅ Follow An Anti-Inflammatory Diet
An anti-inflammatory diet is critical for improving stomach acid levels and reducing heartburn. Try to avoid refined sugar, artificial ingredients, deep-fried food, gluten, dairy, soy, peanuts, corn and refined vegetable oils and processed foods.
Most people notice a reduction in acid reflux symptoms when they eliminate these foods from their diet.
✅ Limit Carb Intake
Certain carbohydrates, especially refined carbohydrates and sugars, tend to be common triggers for acid reflux. Low-carb diets can also lead to weight loss, which can reduce pressure on the stomach.
✅ Try Apple Cider Vinegar (ACV)
Mix 1-2 tbsps of ACV in a cup of water and drink about 10 minutes before each large meal. ACV has natural acetic acid that helps reduce the pH (acidity) of the stomach environment and activates the vagus nerve which turns on the production of stomach acid, bile and pancreatic enzymes to digest food more effectively.
✅ Make Positive Lifestyle Changes
There are many simple ‘life hacks’ you can try: use blocks to raise the head of your bed four to six inches (to help keep acid in the stomach), avoid overeating (smaller portions), don’t eat late at night, be sure to chew your food properly to aid digestion.
✅ Reduce Stress
Chronic stress and poor sleep can lead to inflammation in your body and interfere with your digestion to increase your risk of heartburn. To improve your stomach acid levels naturally, it is important that you reduce stress and improve your sleep.
Develop a nighttime routine that works for you. Stay away from electronics, stressful activities, and food several hours before bed. Sip on herbal tea and wind down with relaxing activities. Aim for 7 to 9 hours of sleep each night.
✅ Consider A Liver Detox
Improve your liver and gallbladder health by following a personalised Nutrition and Lifestyle Action plan and/or detox programme. Reducing the burden on your liver can contribute to improved digestion and a balanced production of stomach acid, alleviating acid reflux symptoms.
Book a Free Discovery Call
Speak to one of our expert practitioners to find out how we can help you treat acid reflux.

YOUR HEALTH. YOUR CHOICE.
While PPIs can be effective at providing short-term relief for acid reflux, natural strategies offer a more holistic approach with long-lasting effects. Embracing a balanced and mindful approach to nutrition and making simple lifestyle changes not only aids in symptom prevention but also promotes a healthier digestive system. Remember, it’s essential to consult with a doctor or functional medicine nutritionist for personalised advice, particularly if you have been taking PPIs.
At Nutrition Diets, we specialise in restoring gut health using the functional medicine approach: 1) expert one-to-one therapy; 2) personalised nutrition and lifestyle plans; 3) easy, at-home functional testing.
We offer thorough clinical assessment via convenient online consultations. Getting started is simple and free. Take action today to get your health back on track.
