Small Intestinal Bacterial Overgrowth, also known as SIBO, is a common gastric condition that we are coming across increasingly often in our clinic. Often associated with IBS, SIBO is frequently implicated as the cause of chronic diarrhoea and malabsorption. Identifying and assessing SIBO is essential as it can cause or exacerbate other gastrointestinal conditions and have far-reaching impacts on your digestive and overall health.
So what exactly is SIBO? And could it be the reason you’re experiencing bloating, diarrhoea and stomach ache?
In this blog, we’ll explore the underlying causes of SIBO, the different types of SIBO and how to identify them with functional testing, and functional medicine strategies that treat SIBO by restoring balance to the microbiome and healing the gut.
An estimated 13 million people in the UK suffer with IBS, a digestive problem that can have a profound impact on quality of life. It is further estimated that as many as 80% of these (up to 10.8M people) have SIBO, and that an even larger number of people suffer from food intolerances.
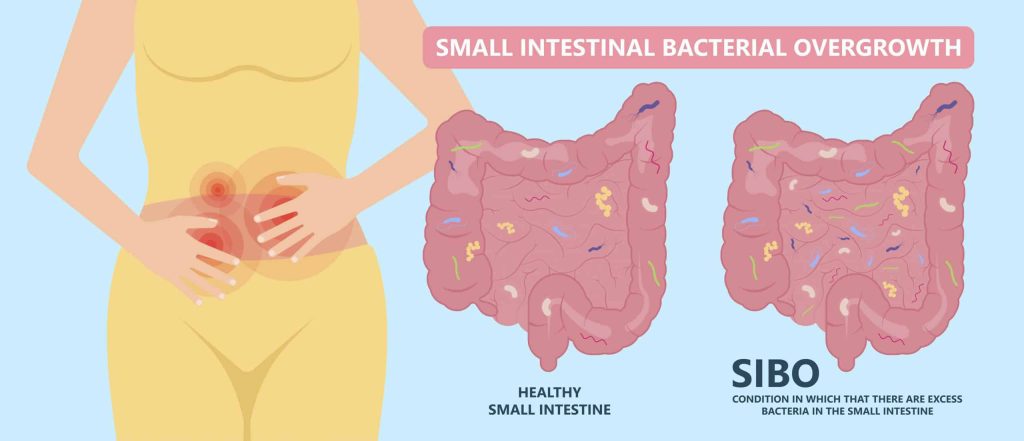
What Is Small Intestinal Bacterial Overgrowth (SIBO)?
In a healthy small intestine – whose primary function is to digest food and absorb nutrients from it – only a small amount of bacteria will be present. SIBO occurs when there is a presence of an excessive amount of bacteria in the small intestine.
The overgrowth of bacteria create more gas than usual during the digestive process which in turn can trigger diarrhoea and uncomfortable digestive symptoms. The excess bacteria also consume proteins, vitamin B12, and bile salts which are meant for digestion and absorption. This results in immediate gastrointestinal symptoms and, over time, contributes to malnutrition, which can have damaging effects on the body.
What Causes SIBO?
Bacterial numbers in the small intestine are maintained by several homeostatic mechanisms including:
- Stomach acid and pancreatic/biliary secretions: which help suppress the growth of ingested bacteria) Factors that may reduce your stomach acid levels include:
- Gut immune function: which helps your intestinal immunity to certain bacteria)
- Small intestinal motility and integrity: which helps the passage of waste into the large intestine)
SIBO develops when these mechanisms are disrupted, resulting in an imbalance in the gut microbiome, commonly referred to as dysbiosis. SIBO can be triggered by multiple factors such as food poisoning, an infection of Helicobacter pylori (H. pylori) bacteria, prolonged usage of medications like antibiotics or gastric antacids, or one of the many reasons for poor motility of the small intestine.

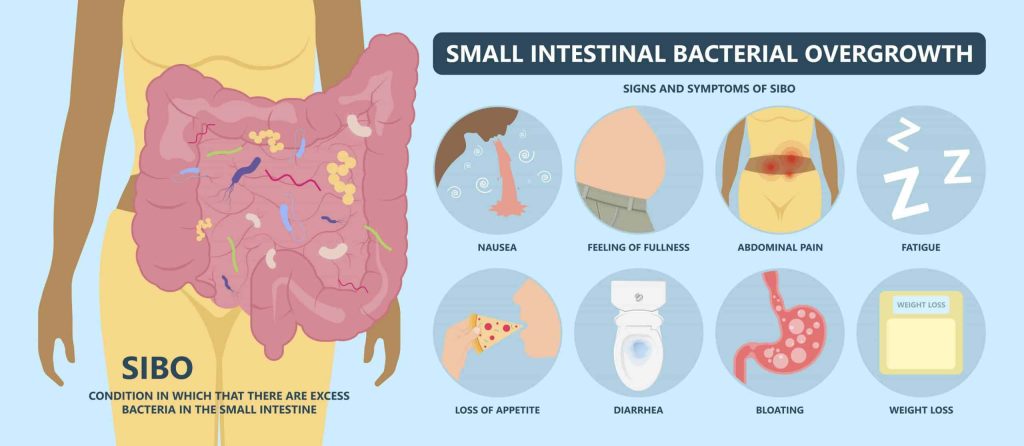
What Are The Symptoms Of SIBO?
SIBO is a multifaceted gastrointestinal disorder and as such is often under diagnosed or mistaken for another gastrointestinal condition. SIBO can manifest through a diverse array of symptoms which can vary in intensity and duration:
- Bloating/distension
- Constipation
- Diarrhoea
- Fatigue
- Gas
- Halitosis (bad breath)
- Indigestion
- Loss of appetite
- Stomach ache
- Stress
- Uncomfortable feeling of fullness after meals
What Other Conditions Are Associated With SIBO?
SIBO is often associated with various conditions, including but not limited to:
- Irritable Bowel Syndrome (IBS) – on average 60% of IBS is caused by SIBO
- Coeliac disease
- Fibromyalgia
- Food sensitivities
- Gastroparesis
- Diverticulosis
- Scleroderma
- Metabolic disorders (diabetes, obesity)
- Intestinal adhesions
- Previous gastrointestinal surgery
These conditions can contribute to the development or exacerbation of SIBO.
What Are The Different Types Of SIBO?
There are three main types of SIBO based on the types of gases produced by the overgrown bacteria. The type of gas produced can influence the symptoms and clinical presentation of SIBO, and it also guides treatment approaches. Testing for the specific gas types can help in tailoring personalised interventions according to the specific type of SIBO.
1. Hydrogen Dominant SIBO
Characterised by elevated levels of hydrogen gas.
Streptococcus, E.coli, Staphylococcus, Micrococcus, Klebsiella, Bacteroides, and Peptostreptococcus are strongly associated with hydrogen dominant SIBO.
2. Intestinal Methanogen Overgrowth (IMO)
Characterised by increased levels of methane gas produced by archaea (a microorganism and not a bacteria) hence it is more appropriately referred to as IMO than its previous name methane SIBO.
Strongly linked with IBS-constipation (IBS-C) and Methanobrevibacter smithii overgrowth (archaea) in the colon and small intestine.
3. Hydrogen Sulphide Dominant SIBO
Characterised by increased levels of hydrogen sulfide gas.
Associated with diarrhoea, and presence of Escherichia, Klebsiella, Proteus, and Desulfovibrio in stool testing.
Book a Free Discovery Call
Discuss your health concerns with one of our expert practitioners and find out how personalised functional medicine can get your health on the right track.
How Do I Know If I Have SIBO?
People with SIBO can have symptoms vary in presentation, from being only mildly symptomatic to suffering from chronic diarrhoea, constipation, weight loss, and malabsorption.
If you are experiencing ongoing digestive symptoms consider the following steps to determine whether you have SIBO. Self-diagnosis can be challenging, and it’s important to seek professional guidance for an accurate assessment and appropriate treatment of your symptoms.
 Consult a SIBO Functional Nutritionist
Consult a SIBO Functional Nutritionist
SIBO can be diagnosed by a functional medicine practitioner using a variety of methods. Depending on your individual case, they will recommend the right course of action to get to the root cause of your digestive symptoms and restore your gut health with a personalised therapy plan.
 Clinical Evaluation
Clinical Evaluation
Your functional medicine practitioner will conduct a thorough medical history and case study to understand your symptoms and potential risk factors then recommend testing and personalised plans accordingly.
 SIBO Breath Test UK
SIBO Breath Test UK
SIBO can be diagnosed with a breath test that measures the gases produced by bacteria in the small intestine. Common tests include hydrogen breath tests and methane breath tests.
People don’t usually produce hydrogen or methane gas in their breath unless they have malabsorption issues, so when these gases are identified, it usually means that bacteria in the gut are producing them.
This breath test is a non invasive diagnostic tool for determining if you are suffering from SIBO/IMO and are the most used test to diagnose this condition versus the most invasive and expensive – the small intestine aspirate and fluid culture.
The test measures the amount of hydrogen or methane that you breathe out after drinking a mixture of glucose or lactulose* substrates and water. A rapid rise in exhaled hydrogen or methane may indicate the presence of gas producing bacterial overgrowth in your gut. If your levels are above a certain number, it suggests an abundance of bacteria and it will determine which type of SIBO you have.
*Patients unable to perform the lactulose breath test due to allergy can take the glucose breath test instead.
 SIBO Microbiome Stool Test UK
SIBO Microbiome Stool Test UK
A comprehensive stool test evaluates digestive health and provides insights into the different factors that can contribute to SIBO such as pathogens, inflammation, or imbalances in the microbial flora (dysbiosis).
The biomarkers of this type of test reflect three key areas of gut health:
- Digestion/Absorption
- Inflammation/Immunity
- Gut Microbiome

How Do I Treat SIBO?
Once the presence and type of SIBO have been identified by your functional medicine practitioner, a strategic approach can be implemented to prevent further dysbiosis and begin healing your gut.
Treating SIBO consists of: 1) addressing underlying causes; 2) providing nutritional support; and 3) addressing the bacterial overgrowth.
Antibiotics
Antibiotics play an important role in SIBO treatment, helping to eliminate and reduce bacterial overload and the reversal of mucosal inflammation associated with overgrowth and malabsorption.
However, following any course of antibiotics, restoration of the gastrointestinal tract is vital for your health, as antibiotics, while acute in their impact, do not offer a long-term solution, and can actually further disrupt your gut microbiome.
The personalised functional medicine approach to treating SIBO complements antibiotic use by tailoring your treatment to your symptoms, ensuring you have the right nutrition and lifestyle plan to restore your gut health. This comprehensive approach ensures not only immediate relief but also lasting results in the management of SIBO.
When antibiotics are used to treat SIBO without a functional medicine approach, it is not uncommon for SIBO symptoms to resurface months after completing an antibiotic course, particularly for individuals with underlying conditions predisposing them to SIBO.
Personalised Nutrition Plan
Although specific foods themselves don’t directly trigger SIBO, certain ones can exacerbate the symptoms. That’s why effectively managing and treating SIBO often requires making dietary changes.
Sometimes short-term, highly restrictive, detoxification-style diets are recommended for SIBO, but oftentimes a softer more gradual approach is most suitable; there is no one-size-fits-all approach. Your functional medicine practitioner will design the most appropriate nutrition plan for you depending on your symptoms and medical history:
- FODMAP Diet – given the huge overlap between SIBO and IBS, the low FODMAP diet is often an effective diet. FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are the scientific names for carbohydrates that are more difficult to digest. The low FODMAP diet temporarily restricts these carbohydrates, alleviating symptoms and giving your gut time to repair itself and rebalance the gut flora.
- Elimination Diet – this involves restricting certain carbohydrate heavy foods from your diet to deprive the problematic bacteria of their preferred nutrients. As symptoms improve, these foods can be gradually added back in to see how your system responds.
Balance The Gut Microbiome
Functional medicine practitioners prescribe personalised supplements protocols to be taken in conjunction with food to improve symptoms and restore healthy gut function.
Supplements like L-glutamine, zinc, quercetin, and collagen are known to support gut lining repair, while probiotics enhance the diversity and abundance of beneficial gut bacteria to support the gut microbiome.
On the other hand, prebiotics (which can be good for people with robust gut health) can be potent producers of hydrogen in the gut which is bad news for many people with SIBO.
Diet is likely to become a significant and serious line of treatment or disease management for diseases of the gut – by modulating the gut microbiome.
– Laura Bolte, researcher at The University Medical Centre Groningen (UMCG)
Book a Free Discovery Call
Speak to one of our gut health experts to find out how we can help you treat SIBO.

YOUR HEALTH. YOUR CHOICE.
SIBO Gut Health Experts
Addressing SIBO through the lens of functional medicine offers a comprehensive and targeted approach to restoring your gut health and overall well-being. If you are experiencing IBS-like digestive symptoms, you may have SIBO, and it is important to seek help from a functional medicine practitioner to prevent chronic disease from developing or progressing.
At Nutrition Diets, we specialise in restoring gut health using the functional medicine approach: 1) one-to-one therapy; 2) personalised nutrition and lifestyle plans; 3) easy, at-home functional testing.
We offer thorough clinical assessment via convenient online consultations. Getting started is simple and free. Take action today to get your health back on track.
