High blood pressure (also known as hypertension) is one of the most common — and dangerous — health issues today. In the UK, it’s estimated that 1 in 3 adults have high blood pressure, and many don’t even know it. Hypertension can quietly damage your heart, brain, kidneys, and eyes over time without any obvious symptoms.
But the good news is you can manage — and even reverse — high blood pressure naturally with the right support, lifestyle changes, and a functional medicine approach tailored to your body.
In this blog, we explore the root causes of high blood pressure, how menopause and andropause impact cardiovascular health, Functional tests to assess your cardiovascular risk and how to take back control of your health with natural foods and nutrients to lower blood pressure.
The prevelance of hypertension increases with age, from 9% of adults aged 16 to 44 to 60% of adults aged 65 and over in the UK.
– NHS
What Is High Blood Pressure and Why Is It Dangerous?
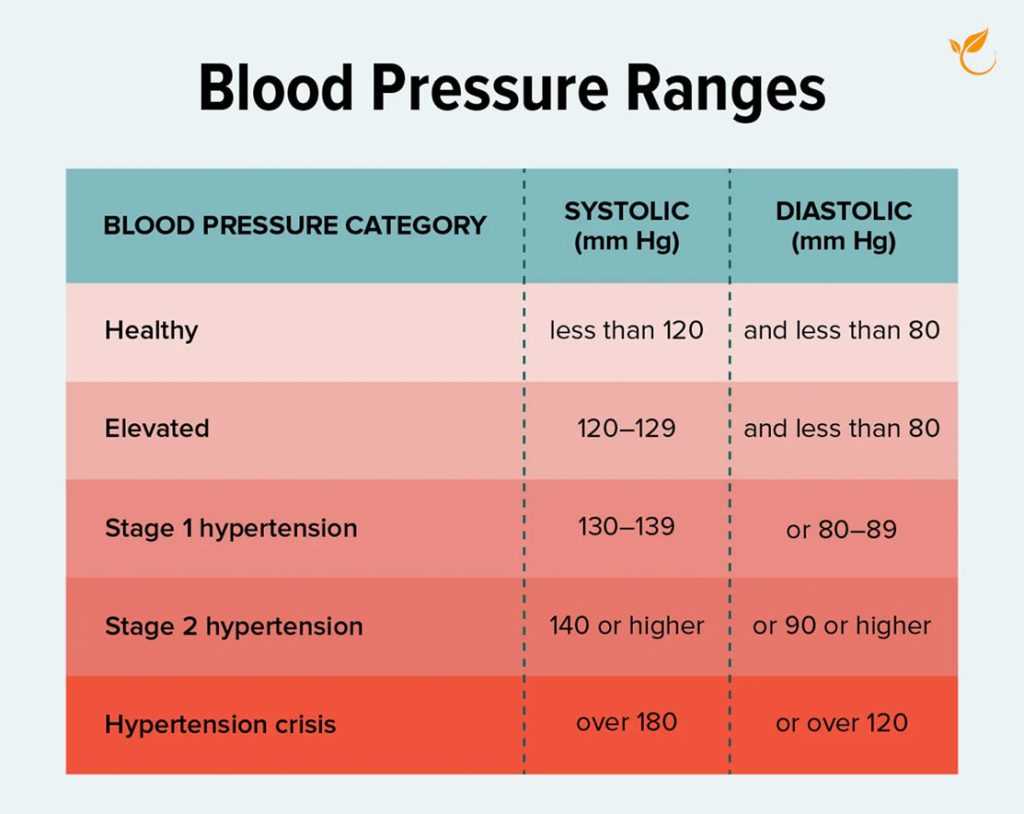
Blood pressure is the force your heart uses to pump blood around your body. A healthy reading is around 120/80 mmHg.
Hypertension occurs when blood pressure is consistently 130/80 mmHg or higher. If left untreated, high blood pressure can damage your blood vessels, increasing the risk of cardiovascular disease and health conditions such as:
- Atherosclerosis (narrowed arteries)
- Cognitive decline and dementia
- Heart disease and heart attacks
- Kidney damage
- Stroke
Book a Free Discovery Call
Discuss your health concerns with one of our expert practitioners and find out how personalised functional medicine can get your health on the right track.
How Do Menopause and Andropause Affect Blood Pressure and Cardiovascular Risk?
While high blood pressure and cardiovascular disease are significant concerns for both men and women, these risks increase substantially with age. For women, menopause leads to hormonal changes that affect heart health, but men also face unique challenges as they age, particularly during andropause, often referred to as male menopause.
How Does Menopause Affect Women’s Heart Health?
During menopause, declining oestrogen levels increase the risk of high blood pressure and cardiovascular disease. Oestrogen normally helps keep blood vessels flexible and dilated, supporting healthy circulation. When levels drop, blood vessels can stiffen, making hypertension more likely.
Postmenopausal women also tend to experience higher LDL (bad cholesterol) and lower HDL (good cholesterol), further raising cardiovascular risk. In fact, a woman’s risk of hypertension doubles after menopause, and heart disease becomes the leading cause of death in postmenopausal women — making blood pressure management especially important during this life stage.
How Does Andropause Affect Men’s Heart Health?
As men age, testosterone levels naturally decline, a shift often referred to as andropause, typically starting in the mid-40s to early 50s. Testosterone supports vascular health, muscle mass, and fat distribution, so reduced levels can lead to increased abdominal fat, insulin resistance, and chronic inflammation — all of which raise the risk of high blood pressure and heart disease.
Over 50% of men over 60 have hypertension, and men are generally at higher risk of cardiovascular disease earlier in life than women, especially with added risk factors like smoking, high cholesterol, or a family history of heart disease.

Functional Medicine Testing for Blood Pressure and Cardiovascular Health
Functional medicine utilises comprehensive and targeted testing to uncover the underlying causes of high blood pressure. Aside from regular blood pressure monitoring, which is essential to track over time, the 10 most common tests we recommend are:
1. Hormone Testing:
For women in menopause and men experiencing andropause, hormone testing can be helpful to assess the impact of hormonal imbalances on blood pressure. Tests can include measurements of oestrogen, progesterone, testosterone, and cortisol levels.
2. Inflammation and Autoimmunity Panel:
Tests like hs-CRP (high-sensitivity C-reactive protein) are used to measure chronic inflammation, a known factor a key factor contributing to both high blood pressure and cardiovascular disease. Elevated CRP levels can indicate inflammation in the arteries, contributing to heart disease and stroke risk.
3. Nutrient Deficiency Test:
Testing for deficiencies in magnesium, vitamin D, potassium, and omega-3 fatty acids can be useful. Low levels of these nutrients have been associated with higher blood pressure and cardiovascular risks.
4. Lipid Profile (Moving Beyond Cholesterol):
Traditional lipid profiles measure LDL, HDL, and triglycerides, but recent studies suggest that very low-density lipoproteins (VLDL) are a more accurate predictor of cardiovascular risk. VLDL particles are smaller and denser than LDL particles, making them more likely to contribute to plaque formation in the arteries. This shift in understanding is encouraging healthcare professionals to assess VLDL alongside other lipid markers.
5. Advanced Lipid Testing:
Beyond the basic lipid profile, tests like Apolipoprotein A1 (ApoA1) and ApoB help assess the number of atherogenic particles and the risk for cardiovascular disease. ApoB, in particular, is a key marker for identifying risk for plaque buildup in arteries.
6. Lipoportein(a) Testing:
Elevated Lipoprotein(a), or Lp(a), levels are associated with an increased risk of heart disease, especially when cholesterol levels appear normal. Testing for Lp(a) can help identify individuals at higher risk, particularly for those with a family history of cardiovascular disease.
7. 24-Hour Urinary Sodium Excretion Test:
This test measures how much sodium is excreted in the urine, which can provide insights into your sodium intake and your body’s ability to manage it.
8. Homocysteine and Vitamin B12/Folate Test:
Functional medicine labs often test homocysteine levels, as well as Vitamin B12 and Folate levels, because deficiencies in these nutrients can lead to higher homocysteine levels, which are associated with an increased risk of heart disease.
9. Methylation and Genetic Testing:
Genetic factors play a key role in cardiovascular health. Tests that evaluate methylation patterns, such as MTHFR gene mutations, can help understand your body’s ability to metabolise folate and other key vitamins. Genetic tests can also offer insights into predispositions to heart disease and how lifestyle changes can be tailored to reduce these risks.
10. CardioMetabolic Panel:
This test evaluates cardiovascular risk markers like cholesterol levels (HDL, LDL, total cholesterol), triglycerides, and other lipid biomarkers. It also looks at metabolic factors that influence heart disease, such as insulin resistance, inflammatory markers, and oxidative stress.
For more information on our range of functional tests, how they work and how you can book a test, visit our Functional Medicine & Testing page.
The Functional Medicine Approach to High Blood Pressure and Cardiovascular Health
Managing high blood pressure isn’t just about medication — in functional medicine, we focus on sustainable, root-cause lifestyle changes that support cardiovascular health from all angles. Below are some of the core interventions we recommend to our clients for blood pressure control.
Keep in mind that each of these strategies can be effective on its own — but when combined and properly managed, they create a holistic, long-term solution to regulating blood pressure naturally.
1. Balance Blood Sugar to Reduce Hypertension Risk
Blood sugar and blood pressure are more connected than most people realise. Insulin resistance (often a precursor to type 2 diabetes) can raise blood pressure by promoting inflammation, increasing sodium retention, and disrupting vascular health.
Nutrition plays a central role in cardiovascular health and blood pressure. Focus on personalised food plans that incorporate foods scientifically proven to support heart health and help reduce blood pressure.
How we help you balance blood sugar:
-
Prioritise low-glycaemic, whole foods like leafy greens, berries, legumes, and healthy fats
-
Include lean protein and fibre in every meal to prevent glucose spikes
-
Reduce refined carbs and ultra-processed foods
-
Use targeted nutrients like berberine, alpha-lipoic acid, chromium, and magnesium
2. Supporting Detox Pathways
Environmental toxins like BPA, phthalates, and heavy metals can disrupt hormones, raise inflammation and damage blood vessels— all contributing factors to hypertension and cardiovascular dysfunction.
How we help you reduce your toxic load by:
- Assessing heavy metal exposure via functional testing (e.g., mercury, lead, arsenic)
- Support liver detox with antioxidant foods like broccoli sprouts, cruciferous veg, garlic, and glutathione boosters
-
Eliminating exposure to toxins in your food and lifestyle and encouraging toxin-free alternatives such as filtered water and BPA-free containers
3. Reduce Stress & Regulate Cortisol
Chronic stress activates the sympathetic nervous system, leading to vasoconstriction (narrowed blood vessels) and elevated cortisol, which can contribute to persistent high blood pressure. We recommend various strategies according to each person’s needs:
How we help you reduce stress naturally:
-
Use adaptogenic herbs like ashwagandha, rhodiola, and holy basil
-
Support the HPA axis (hypothalamic-pituitary-adrenal) with proper nutrition and rest
-
Encourage daily stress relief rituals: meditation, deep breathing, journaling, or nature walks
-
Track and improve sleep, as poor sleep is a major contributor to hypertension
4. Targeted Supplements
Based on each individual’s health history (not a one-size-fits-all approach), we prescribe targeted supplement protocols designed to address the symptoms and underlying causes of high blood pressure. Some of the key supplements we may recommend for cardiovascular support (after assessing test results) are:
-
Magnesium (taurate or glycinate): to support vascular relaxation and stress resilience
-
CoQ10: especially beneficial if you’re on statins or have low energy
-
Omega-3 fatty acids (EPA/DHA): to reduce inflammation and improve endothelial function
-
Garlic extract: for its natural blood pressure–lowering and nitric oxide–enhancing effects
-
Potassium (under supervision): to support sodium balance in those with low dietary intake
5. Move Your Body – Gently & Consistently
You don’t need to run marathons to improve heart health. In fact, overexercising can sometimes increase cortisol and stress the body.
Our movement recommendations:
-
Aim for at least 30 minutes of gentle aerobic activity daily (e.g., brisk walking, cycling, dancing)
-
Include mobility and strength training 2–3x per week to improve insulin sensitivity and circulation
-
Incorporate restorative movement like yoga, tai chi, or Pilates to calm the nervous system
For more information on our personalised health protocols and how you can get started, visit our How It Works page.
Book a Free Discovery Call
Schedule a consultation with our functional medicine expert to uncover the root cause of your symptoms and receive a tailored treatment plan.
YOUR HEALTH. YOUR CHOICE.
High blood pressure doesn’t happen overnight — and the same goes for reversing it. But with the right personalised plan, it’s absolutely possible. Whether you’re navigating menopause, andropause, or simply want to prevent future heart problems, our tailored, root-cause approach puts you back in the driver’s seat.
At Nutrition Diets Clinic, our functional medicine approach goes far beyond generic advice by considering your unique genetic makeup, diet, environmental exposures, lifestyle factors, and health history.
1) Expert one-to-one therapy
2) Personalised nutrition and lifestyle plans
3) Easy, at-home functional testing
Starting the journey towards improved health can feel daunting but our team of qualified professionals are here to provide you with expert guidance and support every step of the way.
We offer thorough clinical assessment and therapy via convenient online consultations. Getting started is simple and free. Take charge of your health today with our evidence-based strategies.
