For decades, salt has been blamed as a major cause of high blood pressure and heart disease, leading to widespread recommendations to cut back on sodium intake. But did you know that sodium plays a crucial role in hydration, nerve function, muscle contractions, and even hormonal balance?
While excessive salt consumption can contribute to health issues, too little salt can also be harmful, affecting everything from your energy levels to your cardiovascular and bone health. The real issue isn’t salt itself but the type of salt being consumed and its balance with other minerals like potassium and magnesium.
In this comprehensive blog, we’ll explore the health effects of salt and provide practical tips and functional medicine strategies for maintaining balanced sodium intake in your diet.
As of 2019, adults in England consumed an average of 8.4 grams of salt per day—9.2g/day for men and 7.6g/day for women. This exceeds the UK’s recommended maximum intake of 6 grams per day.
Salt vs Sodium – What’s The Difference?
Salt and sodium are often used interchangeably, but they are not the same thing. Sodium is a mineral and an essential electrolyte, while salt is a compound that contains sodium:
- Sodium (Na) is a naturally occurring and essential mineral and electrolyte found in many foods (like vegetables, dairy, meat and seafood) and is crucial for nerve function, muscle contractions, and fluid balance.
- Salt (sodium chloride – NaCl) is a chemical compound made up of 40% sodium and 60% chloride. It is the main source of sodium in the diet and is typically added to food for flavour and preservation.
This distinction matters because many processed and packaged foods contain “hidden sodium”, even if they don’t taste salty. Common sources of hidden sodium include bread, sauces, soups, processed meats, and fast food. While some sodium is essential for health, excess intake – particularly from hidden sodium in these kinds of pre-packaged foods – can contribute to high blood pressure and other health issues without you realising that you over consuming it.
Understanding the difference between salt and sodium will help you make informed dietary choices. The goal isn’t to eliminate salt but to opt for natural, mineral-rich sources and maintain a balanced intake.
The Role Of Salt In The Body
Salt is essential for maintaining balance and supporting vital physiological functions. The sodium in salt acts as a key electrolyte, helping to regulate fluid balance by ensuring that water is properly distributed inside and outside of cells. This is critical for hydration, circulation, and preventing dehydration. Sodium also plays a central role in nerve signalling and muscle contractions, allowing the brain to send messages through the nervous system and enabling muscles to contract and relax properly — including the heart.
Beyond hydration and nerve function, salt is crucial for your digestive health. It helps produce hydrochloric acid (HCl) in the stomach, which is necessary for breaking down food, absorbing nutrients like iron and vitamin B12, and preventing bacterial overgrowth in the gut. Sodium also works alongside other electrolytes, such as potassium and magnesium, to regulate blood pressure, kidney function, and adrenal health.
When sodium levels are too low, it can lead to fatigue, brain fog, dizziness, muscle cramps, and even hyponatremia (a condition where the body’s sodium levels drop too low, causing confusion, nausea, and swelling in the brain). On the other hand, excessive salt intake can lead to high blood pressure and water retention.
What Is The Maximum Amount Of Salt You Should Consume Per Day?
The UK’s National Health Service (NHS) advises adults to limit their salt intake to no more than 6 grams per day (equivalent to one teaspoon) to help reduce the risk of cardiovascular disease.
The World Health Organization (WHO) recommends keeping salt consumption below 5 grams per day (equivalent to slightly less than one teaspoon).
For children aged 2–15 years, the WHO suggests a lower intake than adults, adjusted based on their energy needs. However, these guidelines do not apply to infants during exclusive breastfeeding (0–6 months) or the complementary feeding period (6–24 months).
All dietary salt should ideally be iodised, as iodine is crucial for brain development in infants and young children and supports cognitive function and thyroid health in adults. Iodised salt is simply table salt fortified with iodine, an essential mineral that helps prevent iodine deficiency and supports optimal thyroid function.

How Does Salt Affect Blood Pressure & Cardiovascular Disease?
Excessive salt intake is a well-documented contributor to high blood pressure (hypertension). When the body has too much sodium, it retains water to maintain balance, increasing blood volume and pressure on the arteries. Over time, this extra strain can damage blood vessels, increasing the risk of heart attacks, strokes, and heart failure.
While not everyone is salt-sensitive, studies show that reducing sodium intake can significantly lower blood pressure, particularly in individuals with hypertension or those at risk of cardiovascular disease. Maintaining a balance between sodium and potassium intake is also essential for heart health, as potassium helps counteract the effects of sodium.
Conversely, reducing sodium intake has been shown to lower blood pressure and decrease the risk of cardiovascular events. These findings underscore the importance of moderating salt consumption to maintain cardiovascular health.
How Does Salt Affect Kidney Health?
The kidneys play a critical role in regulating sodium levels, filtering excess sodium from the bloodstream and excreting it through urine. However, consistently high salt intake forces the kidneys to work harder, leading to fluid retention and elevated blood pressure.
Over time, this added strain can impair kidney function with research indicating that individuals with higher self-reported salt intake have a significantly increased risk of developing chronic kidney disease (CKD). Those with existing kidney disease are often advised to limit salt intake to prevent further deterioration of kidney function.
Moreover, excessive salt intake may have detrimental effects on glomerular hemodynamics, inducing hyperfiltration and increasing glomerular pressure (blood pressure inside the tiny filtering units in the kidneys known as glomeruli), which can contribute to the progression of kidney disease. Therefore, moderating salt consumption is crucial for maintaining kidney health and preventing CKD.
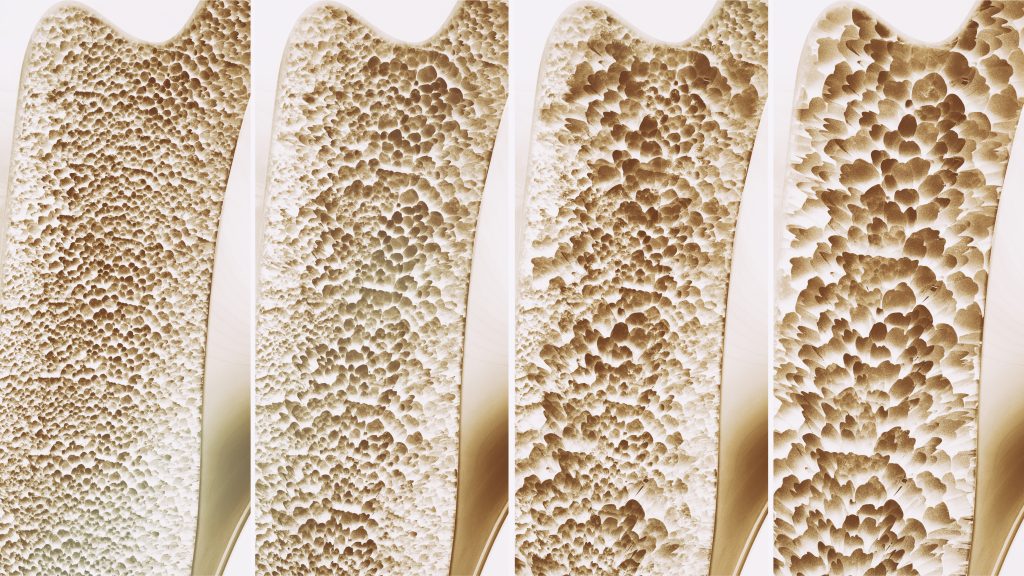
How Does Salt Affect Bone Health & Osteoporosis?
Excess sodium doesn’t just affect blood pressure — it can also have a negative impact on bone density. Studies have shown that high sodium consumption is associated with increased urinary calcium excretion, which may weaken bones over time and increase the risk of osteoporosis (a condition where bones become brittle and more susceptible to fractures).
This is particularly concerning for postmenopausal women, who are already at a higher risk for bone loss due to hormonal changes. Maintaining an adequate intake of calcium and vitamin D while keeping sodium consumption in check can help protect bone health.
However, the relationship between salt intake and bone health is complex, with some research suggesting that low salt diets may also be linked to an increased risk of osteoporosis.
Therefore, maintaining a balanced salt intake that follows the recommended guidelines, along with adequate calcium and potassium consumption, is the best course of action to support bone health.
How Does Salt Affect Stomach Health & Gastric Cancer?
A high-salt diet has been linked to an increased risk of stomach cancer, primarily due to its role in damaging the stomach lining. Excess sodium can lead to inflammation and irritation of the gastric mucosa, making the stomach more susceptible to infection by Helicobacter pylori (H. pylori), a bacterium associated with stomach ulcers and cancer.
Studies suggest that individuals who consume high amounts of salted, processed, and smoked foods are at a significantly greater risk of developing gastric cancer. Reducing intake of processed, high-sodium foods and opting for fresh, whole foods can lower this risk.
How Does Salt Affect Obesity & Metabolic Health?
While salt itself does not contain calories, a high-sodium diet is often associated with processed and fast foods, which are typically high in refined carbohydrates, unhealthy fats, and added sugars — all of which contribute to weight gain and obesity. Excessive sodium consumption may also influence appetite regulation, leading to increased food cravings and overeating.
Studies have found that individuals with higher sodium intake are at an increased risk of developing obesity and central obesity, whilst additional research suggests that diets high in sodium may contribute to insulin resistance, a key factor in type 2 diabetes and metabolic syndrome. Choosing whole, minimally processed foods and cooking at home can help reduce both sodium and unhealthy calorie intake.
Emerging research suggests that excessive salt intake may contribute to obesity and metabolic health issues through several mechanisms. High sodium consumption has been linked to the development of leptin resistance, a condition where the body becomes less responsive to leptin, the hormone responsible for regulating hunger and energy balance. This resistance can lead to increased appetite and weight gain.
Additionally, a high-salt diet may activate the aldose reductase–fructokinase pathway in the liver, resulting in endogenous fructose production. This process can induce metabolic syndrome characteristics, including insulin resistance and fatty liver disease.
These findings highlight the importance of moderating salt consumption to support metabolic health and reduce the risk of obesity-related complications.
How Does Salt Affect Menière’s Disease & Inner Ear Disorders?
Menière’s disease is a chronic disorder of the inner ear that causes episodes of vertigo (dizziness), ringing in the ears (tinnitus), hearing loss, and a sensation of fullness in the ear. Excess sodium can exacerbate fluid retention in the inner ear, which can worsen symptoms and lead to more frequent vertigo attacks.
Individuals with Menière’s disease are often advised to follow a low-sodium diet to help manage fluid balance in the inner ear and reduce the severity of symptoms. Staying well-hydrated and limiting processed foods can further support inner ear health.
Consequently, many healthcare providers recommend a low-sodium diet, typically limiting intake to 1,500 to 2,000 milligrams per day, to help manage the condition.
However, it’s important to note that a Cochrane review found no high-quality evidence from randomised controlled trials to support or refute the effectiveness of salt restriction in managing Ménière’s disease.
Despite the lack of definitive evidence, some patients report symptom improvement with dietary sodium reduction. Therefore, individuals with Ménière’s disease should consult with their healthcare providers to determine the most appropriate dietary approach for their specific situation.
How Does Salt Affect Bloating & Water Retention?
A high-salt diet can lead to excessive water retention, causing bloating and swelling in the face, hands, and feet. This is because sodium pulls water into the bloodstream, increasing fluid retention in tissues. This effect can be particularly noticeable after consuming salty restaurant meals, processed foods, or snacks like crisps.
In some cases, fluid retention can also contribute to puffiness, sluggishness, and discomfort. Drinking plenty of water, reducing sodium intake, and consuming potassium-rich foods (like leafy greens, bananas, and avocados) can help counteract bloating and restore fluid balance.

What Are The Healthiest Types Of Salt?
One way of improving your salt intake is by reducing your intake of table salt – which is heavily processed and stripped of minerals – and instead choosing unrefined, high-quality, mineral-rich types of salt.
Instead of eliminating salt, focus on choosing high-quality, mineral-rich salts. Some of the best options include:
- Himalayan Pink Salt – Contains trace minerals like magnesium, calcium, and potassium that supports electrolyte balance.
- Celtic Sea Salt – Moist, grey-coloured salt with higher magnesium content, great for hydration.
- Redmond Real Salt – Unrefined, from an ancient sea bed, naturally rich in minerals.
Choosing mineral-rich, unprocessed salts over refined table salt helps provide essential nutrients while avoiding unnecessary additives like anti-caking agents.
How to Use It?
- Add a pinch of Celtic sea salt to your morning water for electrolyte balance.
- Use mineral-rich salt in cooking instead of refined table salt.
- Consider an electrolyte drink with salt, potassium, and magnesium if you sweat a lot or experience fatigue.

Book a Free Discovery Call
Discuss your health concerns with one of our expert practitioners and find out how personalised functional medicine can get your health on the right track.
How To Reduce Salt Intake: Functional Medicine Strategies
The good news is that there are many simple and effective steps you can take to reduce salt intake and manage health conditions linked to excessive sodium consumption, both at home and with the guidance of a functional medicine practitioner.
Functional medicine takes a holistic approach to addressing high salt intake and its associated health risks, such as high blood pressure, kidney disease, water retention, and cardiovascular issues. This comprehensive strategy includes dietary modifications, targeted supplementation, lifestyle interventions, stress management techniques, and functional testing. By identifying the root causes of salt-related health conditions and imbalances, functional medicine aims to restore optimal health and prevent chronic disease progression.
1. Nutrition & Lifestyle
Personalised nutrition is at the core of functional medicine. Many of our dietary habits and salt consumption patterns are formed through routine behaviours and food choices made on autopilot.
Working with a functional medicine specialist can help you identify sources of excess sodium, provide healthier alternatives, and tailor a sustainable plan to support your long-term health. Some of the key principles of this approach are:
- Nutritional Interventions – Instead of focusing solely on reducing salt, functional medicine emphasizes mineral balance by increasing potassium-rich foods (such as leafy greens, avocados, and bananas) that counteract sodium’s effects on blood pressure. A diet centred around whole, unprocessed foods — such as vegetables, lean proteins, healthy fats, and high-fibre grains — naturally reduces excessive sodium intake while supporting overall metabolic health.
- Lifestyle Modifications – Regular exercise, stress management, and proper hydration all play an essential role in maintaining healthy blood pressure and kidney function. Functional medicine practitioners often incorporate lifestyle coaching, mindfulness, breathwork, and sleep optimisation into a patient’s plan to regulate stress-induced sodium retention and promote electrolyte balance.

2. Monitoring & Functional Testing
Functional testing can provide valuable insights into how salt is affecting your blood pressure, kidney function, electrolyte balance, inflammation, and overall metabolic health. Here are some of our most popular functional testing options for identifying imbalances and underlying conditions:
- Blood Pressure & Cardiovascular Risk Assessments – High sodium intake is a well-known risk factor for hypertension and cardiovascular disease. Monitoring blood pressure trends, heart rate variability (HRV), and inflammatory markers like C-reactive protein (CRP) can help assess cardiovascular health and guide lifestyle interventions.
- Bone Health & Nutrient Deficiency Tests – Excessive salt intake can increase calcium excretion, leading to weakened bones and osteoporosis risk. Testing for calcium, magnesium, and vitamin D levels can help prevent mineral depletion and support bone density.
- Comprehensive Metabolic Panel (CMP) – A CMP test assesses kidney function, blood sugar levels, and liver health, which can all be affected by excessive salt intake. Poor kidney function can lead to sodium retention and high blood pressure, making this test essential for monitoring long-term effects.
- Electrolyte Panel & Sodium Testing – This test measures sodium, potassium, and chloride levels to evaluate electrolyte balance and detect sodium imbalances that may contribute to hypertension, kidney dysfunction, or dehydration.
- Gut Health & Microbiome Testing – Emerging research suggests a link between high-salt diets and gut dysbiosis (imbalanced gut bacteria), which can contribute to inflammation, metabolic disorders, and poor digestion. A stool analysis or microbiome test can help determine how dietary salt may be affecting gut health.
- Inflammatory Markers & Kidney Function Tests – Chronic inflammation and kidney dysfunction can be exacerbated by excessive salt consumption. Functional testing for C-reactive protein (CRP), interleukin-6 (IL-6), and creatinine levels helps assess systemic inflammation and kidney health.
- Thyroid Function Tests – The thyroid plays a key role in metabolism and fluid balance, and excessive salt intake—particularly iodized salt—may impact thyroid hormone levels. Testing for TSH, Free T3, and Free T4 can help assess thyroid health and its connection to sodium metabolism.
- Urine Sodium & Aldosterone Testing – This test helps measure how much sodium your body is excreting, which can indicate whether your kidneys are properly regulating salt balance. It also evaluates aldosterone levels, a hormone that controls sodium retention and blood pressure.ws for targeted supplementation to improve glucose control and insulin sensitivity.
For more information on our range of functional tests, how they work and how you can book a test, visit our Functional Medicine & Testing page.
Book a Free Discovery Call
Speak to one of our trusted practitioners to find out how we can help you reduce your sodium intake, as well as manage a variety of health conditions associated with overconsumption of salt.
Practical Steps For Reducing Salt Intake
Reducing salt intake doesn’t mean sacrificing flavour or enjoyment — it’s about making smarter food choices and adopting healthier habits. Try following these practical steps for the next 7 days and see how you do:
1. Minimise Processed & Packaged Foods
These often contain high levels of hidden sodium in preservatives, sauces, and seasonings.
2. Choose Fresh, Whole Foods
Instead of pre-packaged foods, opt for fruits, vegetables, lean proteins, and whole grains, which naturally contain lower sodium levels.
3. Cook At Home More Often & Avoid Take-Away Foods
Cooking at home allows you to control how much salt is added to meals, making it easier to stick to healthy sodium guidelines.
4. Limit Sauces & Condiments
Many sauces, dressings, and condiments are high in sodium. Opt for low-sodium versions or use them sparingly.
5. Check Nutrition Labels When Food Shopping
Reading nutrition labels and choosing “low-sodium” or “no added salt” versions of products can help reduce overall intake without compromising flavour.
6. Increase Potassium-Rich Foods
Leafy greens, avocados, and bananas) helps counteract the effects of sodium on blood pressure. Staying hydrated and avoiding excessive consumption of salty snacks, fast food, and processed meats can further support a balanced sodium intake.
7. Remove The Saltshaker From The Table
Get into the habit of tasting your food first before adding salt. You’ll be amazed at how good food tastes in its natural state and learn to appreciate its true flavour without enhancing it too much.

Around 75% of the salt we eat comes from packaged and everyday foods we buy, such as bread, breakfast cereals, meat products and ready meals.
– NHS
YOUR HEALTH. YOUR CHOICE.
Managing salt intake is not just about restriction — it’s about balance, awareness, and making informed choices that support long-term health.
At Nutrition Diets Clinic, our functional medicine approach goes far beyond generic advice to consider your unique genetic makeup, diet, environmental exposures, lifestyle factors, and health history:
1) Expert one-to-one therapy
2) Personalised nutrition and lifestyle plans
3) Easy, at-home functional testing
By understanding your body’s individual needs and applying evidence-based functional medicine strategies, you can optimise your sodium intake, reduce the risk of salt-related health conditions, and promote lasting well-being.
We offer thorough clinical assessment and therapy via convenient online consultations. Getting started is simple and free, so why not take charge of your health today with our evidence-based strategies?
